|
Eggs, salmon, lettuce, asparagus. All healthy foods, they also can be a cause of inflammation. How can this be? And could you have food inflammation to even the healthiest of foods? It’s a big topic in the functional medicine world today, and every day there is new research coming out about it.
As a functional medicine practitioner, I run food inflammation tests on just about every client of mine and have discovered some surprising things throughout the years. First things first, let’s talk about what food inflammation really is. What is Food Inflammation? Most people understand what a food allergy is, but food inflammation is a much newer concept that many are just starting to hear about. Let’s first look at what happens when someone has an allergy to peanuts, as an example. If allergic, immediately upon eating a peanut, someone can experience an anaphylactic reaction, such as swelling of the throat or tongue and even shortness of breath or vomiting. This is because the antibody produced by your immune system called Immunoglobulin E, or IgE, is detecting a food that doesn’t work for that person and causes a serious and quick response. Food inflammation, on the other hand, doesn’t create such an immediate or noticeable response. Oftentimes, reactions take from one to seven days to show up. That’s because food inflammation is mediated by a different Immunoglobulin called IgG, which causes a delayed response. Another term called food sensitivities is also mediated by IgG, however they are often prone to false positives as they are measured in a different way, as we explain in the following section. In our experience running these tests in our practice, not only do common inflammatory foods like dairy and wheat often show up on a food inflammation test (or FIT), but foods we consider very healthy can also create inflammation. This can result in fatigue, aches, stomach pains, reflux and even rashes. But it’s extremely difficult to detect which foods are causing these reactions without running a food inflammation test because the response can be far removed from when a food was consumed. The Most Effective Way to Test for Food Inflammation Here at Pioneer Health Center, we run the most advanced food inflammation test that we know of. After years of research on the subject, and evaluating different methods of measuring food inflammation, we selected the one we believe gives the most accurate recording. The scientists who created this lab-administered blood test determined a very specific way to detect if the response to a food antigen was truly inflammatory or not, a process which greatly reduces the presence of false positives. When there is a true food inflammation response in the body, not only will the IgG complex be present, but a complement protein will also bind to this complex, confirming the inflammatory response. So, by detecting when the complement protein binds to the IgG antibody, we can verify food inflammation. Other tests, such as food sensitivity tests, just look for IgG to be present, but this doesn’t tell the entire story and may not be indicative of a true food inflammation response. IgG antibodies can show up for a number of reasons, but not always because there is an inflammatory response to a food. In this way, food inflammation can be a much more precise way of identifying immune reactions to food. What’s more is this detection capability works not just on food proteins, but food additives as well. This means we can detect if a person is reacting to food colorings or flavorings, which are present in a large majority of foods today. This allows us to get hyper-specific about a patient’s dietary needs once we know what their body can’t tolerate and what it can. How Food Inflammation Occurs If you think about it, our digestive tracts interact on a regular basis with our outside environment. Everything we are exposed to physically, so too is our digestive tract. Did you know that the cellular structure that lines this pathway and separates the outside world from our inside world is only one cell thick? Picture this: There is a row of bricks lined up one-by-one. Holding them together is the mortar, which seals up the gaps between the bricks. If the line of bricks is hit by something, it can begin to rupture, letting unwanted things in. This is exactly what happens in our digestive tracts when we are exposed to toxins from our environment, and can lead to a condition called “leaky gut”. With leaky gut, the area between those bricks (or our cells) begins to widen and allows antigens and undigested proteins to get past the barrier and inside our bodies. Just past this barrier (which, remember, is only one cell thick) are most of our immune cells. These cells are here to defend against potential invaders like chemicals and food antigens. Essentially any substance that passes through this barrier that the immune cells don’t recognize as normal (even the healthiest of foods), it views as an invader and launches an immune (IgG) response against it to try and remove it from the body. As a result, food inflammation occurs (and is confirmed only when the complement protein is present as well). Inflammation is our body’s primary immune response. If you think about what happens when you sprain your ankle, it gets inflamed. The same happens when our immune cells interact with a “foreign” substance. It’s important to note that this process can happen with any kind of food, healthy or not. If the digestive tract is damaged from triggers like pollution, processed foods, or medication (more on that below), and a person eats a food regularly enough, chances are high it’s going to come in contact with this compromised barrier, passing through the threshold and meeting the immune system. Most often when we run food inflammation tests, we see clients come up positive for healthy foods they eat every day. But who would have thought that healthy foods could participate in creating inflammation and degenerative conditions like autoimmunity and mental disorders in people? What Causes Food Inflammation The occurrence of food inflammation is rising at an alarming rate because of the decline in quality of our environment and our body’s attempt to compensate and react to it. In our experience, food inflammation is most often triggered by the environment that we’re exposing ourselves and our digestive tracts to. If exposure is prolonged, it can lead to dysbiosis, or an alteration or manipulation of bacteria in our digestive tracts — and not in a good way. Here are the main contributors to gut dysbiosis and food inflammation: Antibiotics - One of the biggest culprits of food inflammation that we see today is antibiotics. This isn’t referring only to the ones we take orally, but antibiotics that the food animals we eat are given, too. Most antibiotics produced in this country today are in fact for animals, not humans, so in theory, a person could never take an antibiotic pill yet still get exposure to it through food, which can potentially lead to damage in the gut, and eventually, food inflammation. Pesticides and Herbicides - Pesticides and herbicides are two other major contributors to dysbiosis, and as a result, food inflammation. Unless someone has eaten food only from a trusted organic source their entire life, they have had exposure to these toxic but common chemicals. And that can have an enormous effect on the microbiome. Lack of Nutrient-Dense Foods - The quality of food today is vastly different from what it was just a decade or two ago. Declining soil and air quality, coupled with the use of pesticides, herbicides, and other toxic chemicals, has altered the structure and nutrient density of foods ranging from potatoes to kale to blueberries. Without enough nutrients in our bodies to keep our cells strong and able to defend against pathogens and foreign substances, we can succumb to infections, oxidative stress, and damage to the digestive tract. Food Alteration - It is estimated that up to 75 percent of the world’s population has a dairy sensitivity today. In our research and clinical experience, this is most often due to the process of pasteurization where dairy molecules experience an actual change in chemical structure. A similar process has happened with wheat. Most wheat today is also highly modified, so much so that it doesn’t even look like the wheat produced 50 years ago. When a food is changed to this extent, our bodies no longer recognize it, and our immune systems view it as a foreign entity that doesn’t belong in the body. Because of these common triggers, we have yet to come across a food inflammation test that comes up completely negative… Why Everyone Should Run a Food Inflammation Test As I touched on earlier, food inflammation doesn’t always create a symptomatic response, or at least not immediately. At Pioneer Health Center, we have been running this food inflammation test on both symptomatic and otherwise healthy individuals and there hasn’t been a single person we’ve run this test on that hasn’t had foods that show up that are creating inflammation. Because of the environment our digestive tracts are exposed to, everybody has some level of food inflammation, but it’s impossible to pinpoint to what unless a food inflammation test is conducted. By removing these foods from the body for a period of time, we remove the inflammatory burden on the body and improve the health situation of the patient overall. Symptomatic patients absolutely feel better, and those who weren’t symptomatic also notice an improvement in their overall wellbeing, perhaps in ways they didn’t even realize were suboptimal. What Happens When Food Inflammation Go Undetected? Food inflammation can lead to some serious degenerative conditions ranging from autoimmune diseases to chronic pain and even accelerated aging. If food inflammation is left unaddressed, a patient may experience increased inflammation overtime, and eventually, the scale may tip and a major health condition can ensue. In our clinical experience, just about every condition in the body is made worse when inflammation is elevated, so in that lens, it’s crucial to identify and remove these during any kind of healing process. In effect, addressing food inflammation opens the door for every single person to improve their health. New and existing patients of Pioneer Health Center can run our food inflammation test in any of our programs. We’d love to talk to you to discuss how pinpointing food inflammation can help to address chronic or unexplained health issues and how we can help you address them all in one of our many programs. Apply to work with us today and we’ll be in touch so that you can schedule a free 15-minute consult with our medical team to discuss how we can best address your health needs.
1 Comment
Functional medicine, holistic health, integrative medicine. Popular terms these days, functional medicine bears a deeper level of understanding as it incorporates all of these principles. That’s why so many people are turning to this approach to healthcare to find answers to their complex and long-standing health concerns.
Unlike conventional or Western medicine, where a group of common symptoms and test results are used to define a condition or “diagnosis” resulting in predetermined therapies (most often a prescription drug), functional medicine is a practice of evaluating the many modifiable factors that are related to the cause of the symptom or condition. Functional medicine views the body as a complex, adaptive system in which one biological function affects another…and another after that. In other words, we don’t believe that anything happens in the body in isolation; the body is, in fact, an interdependent part of a whole that has an effect on the whole. The functional medicine approach enables us to identify harmful components of our lifestyle such as foods that cause inflammation or toxins we are exposed to and then introduce necessary nutrients through diet and supplementation to support the function of the body. Seeing the body in this way, rather than in isolated systems, we have a new lens through which we can interpret, organize, and address complex health issues. By taking a root-cause approach to health care, we can actually begin to find ways to reverse disease, support function, and return the body back to health using diet and lifestyle changes. Reframing Medical InterventionsIn functional medicine, we don’t — and can’t — just look at symptoms to offer us clues. Symptoms are the very last step in the process of dis-ease, meaning a deeper imbalance is often at play in order for that symptom to show up. Let’s take acid reflux as an example. Looking at the symptom alone (heartburn), we could tell a patient to take Pepto Bismol, Tylenol, or Zantac and call it a day, but we don’t do that. Acid reflux can be brought on by gut pathogens like parasites or bacteria, food sensitivities, a melatonin imbalance and even low stomach acid. Following the principles of functional medicine, we look at the details of a patient’s health history and correlate that with the function of their systems by running advanced lab tests. This enables us to find the underlying stressors and triggers that are at play so that we can address those. Taking this approach, upstream symptoms like heartburn often fall away on their own. Utilizing Evidence-Based InterventionsIn the functional medicine model, we begin working with patients at the cellular level. If we can understand what’s happening to the cells themselves (whether that be inflammation, oxidative stress, or immune dysregulation), we can develop deep-rooted treatments. At the cellular level, there is a great level of evidence-based, peer-reviewed and unbiased research, which offers us tremendous opportunity to develop lifestyle-based treatment options related to the cause of the imbalances rather than just using a pharmaceutical designed to treat the effect of the imbalance. As the main functional medicine practitioner here at Pioneer Health, I am continuously searching for the latest research in all fields of healthcare that offer this level of data. Databases like the National Library of Medicine are my go-to resources, and every year I attend multiple conferences in various fields such as compounding pharmacy, Alzheimer’s, autoimmune conditions, genomics and pain management to continue my passion for education. I search out and meet some of the brightest and most progressive practitioners, researchers, and scientists in this rapidly evolving field we call functional medicine. Patient Education is the Primary FocusHow many times as a patient have you walked out the door of your healthcare practitioner’s office scratching your head because you didn’t get the answers you needed about your health concerns? That’s because the insurance-based, conventional medicine model is designed in such a way that allows patients a mere five-minute window of time with their well-meaning doctor, and that’s not a lot of time to cover a lot of ground. Functional medicine practices like Pioneer Health Center bypass insurance altogether, which allows us to be in control of our time and the way in which we can support patients. Instead of five-minute appointments, we give each patient an appropriate amount of time, from 15 minutes to 90 minutes or more depending on the patient’s needs. In this time, we’re gathering the appropriate information and then educating them about what’s going on in their body and how making uniquely targeted diet and lifestyle modifications can shift the terrain and help them recover. We believe information is power, and the more they know, the more they can manage their health. And the more support they get, the more likely they will be to comply with the treatment plan. With the Patient’s Best Interest in MindIn functional medicine, we’re focused on treating the whole patient, the whole time. That means we work with them, gaining insights into their health history and then running advanced lab tests to understand the current state of their health. When we partner with our patients in their health journey, we can gain a far more comprehensive view of the whole person. This level of care, in our experience, offers the greatest chance of preventing and reversing disease, because the patient is involved in the process, and we as practitioners have the best chance to gather the necessary information we need to formulate a customized treatment plan. Every day, patients walk out of our practice, and many other functional medicine practices, healthier than they came in. This is why I believe functional medicine is the medicine of the future and the good news is… it’s already here! Functional Medicine: A Sound Solution to Today’s Epidemic Health CrisisWithout a doubt, medications for acute health issues can save lives, and functional medicine is not against medication. Instead, we believe in making sound and sensible use of prescriptions only when necessary. As a Compounding Pharmacy practice, we, of course, believe in and know the power of medicine and we see how customized medication improves the outcomes of our patients’ health every single day. However, whereas conventional Western medicine seeks to diagnose and manage chronic degenerative disease, functional medicine guides us to gain a complete view of the whole person, not just organs, systems, or symptoms, but the whole system. This, as we mentioned before, allows us to look beyond surface-level symptoms and discover true healing opportunities that medication often can’t address, or at least not on its own Work with UsPioneer Health Center is currently accepting patients to our programs, which you can view here. We would be honored to partner with you in your health journey and give you the full experience of functional medicine. View our programs here and apply today! What is Functional Medicine? Here’s What You Need to Know Pioneer Health Center started as a compounding-only pharmacy back in 2002, and while not a new concept, many people aren’t familiar with what it is exactly. While conventional pharmacy takes a one-size-fits-all approach to medicine, pharmacy compounding takes into account an individual’s unique requirements and is able to actually customize medication for a person to suit their needs. This singular approach to medicine is what drew our team to compounding many decades ago, and in our 15 years of prior conventional pharmacy experience, we never saw the positive results that we’re seeing with patients today.
As the Professional Compounding Center of America (PCCA) explains it, “Pharmacy compounding is the art and science of preparing personalized medications for patients. Compounded medications are made based on a practitioner’s prescription in which individual ingredients are mixed together in the exact strength and dosage form required by the patient.” Put more simply, our goal is to improve the benefit of a medication while reducing the risk of side effects. Pharmacy Compounding is Patient-Specific- Pharmacy compounding makes it possible for a medication to be completely customized to meet an individual’s needs — no matter how complex. Every person has a slightly different metabolism, and this can determine how much or little of an ingredient they can tolerate. For example, we develop many bio-identical hormone replacement therapy (BHRT) creams for both men and women, but we first need to collaborate with a practitioner in order to determine which hormones and at which strength each individual can benefit from by running various hormone tests. Once we know exactly where the patient needs support, we can then compound a specific medication for them. Not knowing this information can hinder patient progress, which is why compounding is especially applicable in scenarios like BHRT. Compounding also enables us to make medications free from the most common problematic ingredients like dairy, gluten, soy, or eggs, so we can reduce or eliminate common adverse effects and maximize the effectiveness of a medicine. We can also customize the way in which a medication will be delivered depending on how the patient can take it. For example, many medications can be compounded into an easily administered flavored suspension for babies. We can also create troches, lollipops, gummies, creams, nasal sprays, and even specially flavored medicines for pets to accommodate even the most unique needs. Pharmacy Compounding Requires a Triad- Pharmacy compounding requires a tight-knit partnership between a patient, practitioner, and compounding pharmacist. We like to call this the “triad”. This allow us to go beyond the “one-size-fits-all” model of conventional medicine to build customized therapies based on a patient’s health history, unique metabolism, and needs. Working with both a practitioner and patient, we can uncover what those exact needs are so that we can greatly increase the chances that a medication will work. At Pioneer Health Center, we work alongside many of our prescribing practitioners and are available to our patients if there are ever any questions about a prescription or its usage, because we genuinely care about successful clinical outcomes. A regional pharmacy, we care about the well-being of our community and it’s our passion to see them feel better. Pharmacy Compounding is personalized medicine. When medically necessary, medications can be incredibly helpful in treating both acute and complex conditions in both humans and animals. For example, one area we specialize in is compounding medications for pain management. Upon a complete health assessment, we can pinpoint the type or types of pain a patient is experiencing, which allows us to work with patients and practitioners to choose the most appropriate medicines to be used for transdermal therapy. This entire process is designed to reduce the risk of side effects while increasing the amount of pain relief. And here at our compounding pharmacy in Connecticut, every ingredient is pure, pharmaceutical grade, and from FDA regulated facilities. This allows us to choose the very best ingredients for our patients. Our standards at Pioneer Health Compounding Pharmacy are among the highest in the industry using some of the most progressive equipment and process validation including outside potency verification. Come visit us today at our store location in Vernon, CT or book an appointment to talk about how we can help you or your patients receive customized and safe medications.
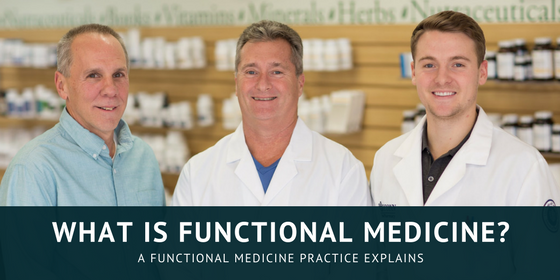
This month, I was interviewed on the LDN Radio Show alongside a good friend and colleague, Dr. Nicholas J. Palermo, to discuss a compounded pharmaceutical that’s proving to be one of the most promising treatments for inflammatory conditions ranging from Crohn’s to fatigue to chronic pain: Low Dose Naltrexone (LDN).
Among the first pharmacies to compound low-dose naltrexone (LDN), we’re also one of the top researchers on it and have worked with over 400 patients taking LDN with incredible results. I was honored to be invited onto the LDN Radio Show. In the interview, we discuss:
LDN is an incredible tool, and what interests us most about it is that it’s not a band-aid approach. LDN actually addresses a foundational cause of inflammation and chronic health conditions, a process which we explain in our full blog post here.
I am actively lecturing on LDN at many schools and universities and welcome the opportunity to speak to your organization as well. Contact us here to find out more about my speaking engagements. Recently I was invited onto the HealthyChoicesXM radio show for a special episode on longevity and healthy aging. Specifically, I was asked to speak about how the compound Synapsin, a patent-pending blend of ginsenoside Rg3, nicotinamide riboside, and an ultra-low dose of Naltrexone, is playing an incredible role in brain health and rejuvenation.
In the interview we discuss:
Synapsin is a safe and highly effective compound that supports healthy aging by decreasing inflammation, a major known source of brain health conditions. We were excited to be one of the first compounding pharmacies to begin using it, and are continuing to research and use it to this day. To learn more about how Synapsin works and who makes a good candidate for it, read our full post. I am actively lecturing on Synapsin at many schools and universities and welcome the opportunity to speak to your organization as well. Contact us here to learn more about my speaking engagements and availability. Traumatic brain injury (or TBI), many of which result in concussions, are a big and rapidly growing problem today for youths and adults alike. Nearly 3 million emergency department visits each year are due to TBI, and of that, 330,000 of them are children being treated with sports-related concussions. With 1 in 5 high school athletes sustaining concussions each season and 33 percent of those having two or more in the same year, we’re reaching an epidemic which can have lifelong repercussions.
Traumatic brain injury is a major focal point of our research here at Pioneer Health Center, and what we’re learning about it is truly groundbreaking. In this post, I’d like to share with you how TBI occurs and how athletes are seeing incredible recovery rates with the compounded preparation, Synapsin. Brain Trauma and the Inflammation CascadeWe used to believe that most neurodegenerative conditions resulted in permanent damage to the brain, but we now understand that it may not actually be damage, but more like a “switch” that’s turned off due to a hit or blow to the head or even inflammation. You see, in a healthy brain, neuron cells (the live tissue in our brain) are constantly being regenerated as others are broken down. But in the case of TBI, a switch is turned off and the scale tips towards neuron breakdown rather than neuron generation. When this happens, this is part of an inflammatory cascade, as it’s a protective measure by the body when damage or a threat is detected. Much like how your ankle swells when sprained, a similar process happens in the brain due to a concussion. In the brain, TBIs can contribute to neurodegenerative conditions like Alzheimer’s disease, dementia, Parkinson’s disease, and behavioral changes, as well as recurring headaches, migraines, and fatigue. Our current research shows that if we can turn this switch back on, we may, in fact, be able to restore normal brain function by reducing inflammation, which is at the core of most TBI-related conditions today. What it comes down to is understanding if our brains are firing signals appropriately or not. When we look at traumatic brain injury in this lens, we can ask ourselves if it’s damage we’re looking at or if it’s actually an incorrectly set switch. If we can help the body more appropriately turn this switch on and off, we can influence healthy physiology and retain function, thus impacting neurodegenerative conditions and chronic concussion damage. Brain on Fire: The Role of Glial CellsTo better understand how our brain operates and why inflammation in the brain occurs due to TBI, we have to look at what are called glial cells. Glial cells are a big topic in neurodegenerative disease research today and were discovered just in the last ten years. Our current understanding is that glial cells play a significant role in neural degeneration (neuron death) and immune cell activation in the central nervous system. With traumatic brain injury, glial cells are immediately activated, creating an inflammatory response. So long as they remain activated, inflammation persists due to the constant release of inflammatory chemicals or mediators. So, what’s activating them? Toll-like receptors, which are receptors designed to look for mediators with either damage-associated molecular patterns (DAMPS) or pathogen-associated molecular patterns (PAMPS). When toxins from the environment or infections like viruses or bacteria are present and detected, the toll-like receptors tell the body there is damage or infection, which activates the glial cells and generates an inflammatory response. Glial cells can also be activated by an imbalance between glutamate and GABA. Glutamate and GABA are like the yin and yang of brain activity. While glutamate is necessary for higher brain function and excitability, GABA allows for rest. We need a balance between the two to have normal brain function, however, trauma to the brain can cause the two to become imbalanced, and may then trigger ongoing inflammation. This can lead to more glial cell activation, keeping the inflammatory cascade going. So, in order to restore balance to the brain, we need to either remove the trigger or block a receptor. This can be especially tricky when someone sustains recurring concussions because of the more frequent the concussion, the more significant the sustained damage due to chronic glial cell activation and inflammation. In cases like this, the brain becomes “on fire”, or constantly activated. As a result, the scale tips towards neuronal death (instead of neuron generation). With this new knowledge about glial cells, we now understand that glial cells may play a role in every degenerative brain or nervous system condition. The good news is, the compounded pharmaceutical, Synapsin, is designed to specifically target glial cells by tipping the scale back into balance. This is true for both acute and chronic concussion and TBI cases. How Synapsin Helps with Chronic Concussion TreatmentThe idea for Synapsin was five years in the making when clinical pharmacist, board-certified nutritionist, and personal friend of mine, Jim LaValle, began using it on athletes with recurring concussions. His initial applications of Synapsin were so rapidly successful that the NFL soon hired him to run a medical facility to help athletes recover from concussions. He found that even athletes who sustained injuries years ago saw remarkable brain function improvements on Synapsin. Additionally, LaValle found Synapsin was having positive effects on those suffering from executive burnout, brain fog, and many other brain-related conditions. So, what exactly is Synapsin? Synapsin is a new and innovative compounded formulation designed to help improve our brain’s ability to decrease inflammation and improve neurogenesis (growth and development of new nervous tissue.) It’s made from a patent-pending powder blend of ginsenoside Rg3, and nicotinamide riboside along with an ultra-low dose of Naltrexone. Specifically, it may support:
LaValle and those of us researching and applying Synapsin are seeing excellent results with people who have concussions or traumatic brain injury because of the way in which it targets the glial cells in this kind of trauma and interrupting the inflammatory cascade resulting in a dampening of the “brain on fire”. Using Synapsin in Functional MedicineAs you may know, not only is Pioneer Health Center a compounding pharmacy, we’re also a functional medicine practice. That means we never look at a medication or health condition in isolation. When we evaluate traumatic brain injury, for example, we know that the body is responding a certain way for a reason. Looking at traumatic brain injury in this way, we can begin to understand what is actually happening in the body and how we can assist it. This is what drew us to Synapsin, because it actually addresses the underlying cause of neurodegenerative disease associated with concussions, as it naturally helps the body balance itself and regain normal function. Today, we’re one of the very first compounding pharmacies using Synapsin and have been seeing incredible results. One of our patients who experienced a concussion and severe memory loss after she fell on ice several years ago reported: “I used to wake up every morning not knowing who I was, where I was, and didn’t even recognize my own mother. Now, since taking Synapsin, I know my name, my home, I recognize my mother, and even my cats!” We’re excited about what this new research means in the field of traumatic brain injury, and that future is already here at Pioneer Health Center as more and more patients come to us for neurodegenerative conditions as well as looking to optimize healthy aging. Contact UsIf you are a physician looking to partner with a compounding pharmacy to offer Synapsin to your patients, or who wants to speak to us more about the applications of Synapsin, contact us today: [email protected]. If you are a university, school, or other organization interested in having us present on the latest TBI research, get in touch with us: [email protected]. And if you are a patient interested in the application of Synapsin, contact us to receive a brochure that you can give to your doctor and discuss if it’s right for you. Autoimmunity is one of the fastest growing health problems today, with over 80 identified conditions and 1 in 5 people currently diagnosed with at least one of them. Conditions like Crohn’s Disease, thyroid disease, multiple sclerosis and more are the result of the immune dysregulation triggered by both external and internal factors, and the effects can be wide-reaching.
As both a compounding pharmacy and functional medicine practice, we at Pioneer Health Center are continuously researching complex health conditions like autoimmunity. One research study in particular sparked our early interest in a compound called low dose naltrexone (LDN). Dr. Jill Smith, a professor at Penn State University, conducted a comprehensive research study on using LDN for Crohn’s Disease and found that patients experienced an 89 percent overall improvement rate and 67 percent achieved remission using this inexpensive compounded pharmaceutical. The impressive results have spearheaded ongoing clinical trials by researchers at institutions worldwide, including right here at Pioneer Health Center. Naltrexone was approved by the FDA in 1984, but prior to Dr. Smith’s study, most of the reports in the literature on LDN were anecdotal and seemed almost too good to be true. Without much science backing the claims, I touted it as a magic pill that would soon be discounted. But when Dr. Smith’s research was published, it validated much of the anecdotal evidence and began to change the face of LDN in the scientific community. I began to research it and have now been compounding LDN for over twenty years. To date, we ’ve worked with over 400 patients taking LDN, and are seeing a widespread positive impact on autoimmunity. How LDN Works in the Body: Multiple Mechanisms of ActionLow Dose Naltrexone is designed to support immune function by upregulating the opioid system in the body. When this happens, endorphin, or “feel good” hormone, production safely increases, which may in turn block inflammatory messengers in the body, thus having a positive influence on immune function and decreasing inflammation. This can also positively impact:
Autoimmune conditions can occur when unusually low levels of endorphins are present, so by stimulating endorphin production, we can effectively modulate correct immune function by stimulating T lymphocyte (or T-cell) production. This has been found to restore a more normal immune response, and as a result, can affect the progress or onset of an autoimmune condition. With such far-reaching effects, it seemed almost too good to be true, but over the last 20 years, scientific breakthroughs and clinical evidence have proven them valid. This is evident in Crohn’s disease in particular, and in our own studies, we found that over 60 percent of our own patients experienced such positive results. Some research even shows that LDN may act directly on immune cells to stimulate or restore normal function by acting as a glial cell modulator, a topic which we explain in detail in this post. In short, glial cells are the immune cells in your central nervous system located in the brain and spinal cord that are involved in the dysregulation of pain, brain inflammation, and neurological diseases like multiple sclerosis, Alzheimer’s, Parkinson’s disease, Autism, ALS, infections of the brain, etc. By calming down over-activation of glial cells, LDN, like Synapsin, may be beneficial in many known neurodegenerative conditions. One of the ways it does this is by blocking what are called toll-like receptors (a concept we explain in-depth in this post), which stops the inflammatory cascade from the immune system from persisting. LDN’s Impact on Thyroid Disease and Multiple SclerosisPatients with thyroid disease and multiple sclerosis often have a strong autoimmune component, meaning Low Dose Naltrexone may be equally effective at addressing it. Using LDN to optimize immune function may lead to a reduction in hypothyroidism and improvement in symptoms when taken for at least 6 months, if not a year or longer. In fact, there are many Hashimoto’s patients who report seeing stubborn thyroid antibodies go down as a result of using LDN, and studies have found that this success is also true for those with Hashitoxicosis–the combination of Hashimoto’s and Graves Disease (TPO) antibodies. There is also significant anecdotal evidence now that supports the benefits of LDN in multiple sclerosis. In fact, one recent study showed that serum Opioid Growth factor levels are lower in those with multiple sclerosis relative to non-multiple sclerosis patients, but LDN restored their levels. The Future of Autoimmunity Looks PositiveDespite the rapid growth of autoimmune conditions today, the promise of Low Dose Naltrexone’s efficacy to improve immune modulation is encouraging. Research continues to demonstrate that LDN is a safe and promising approach to the prevention and/or treatment of many autoimmune diseases, cancer variants and neurological diseases that are due to compromised immunity. And in our own experience, it’s been one of the most beneficial treatments for a wide range of autoimmune diseases. Since LDN can upregulate endogenous opioid activity, it may also have a role in promoting stress resilience, improving emotional states, increasing energy, and positively impacting psychiatric problems including autism and depression. Due to its ability to beneficially modulate both the immune system and brain neurochemistry, it offers a new and positive therapy for millions of patients worldwide. Contact Pioneer Health CenterAs the founder of one of the first pharmacies to begin compounding LDN, and with two decades of research under my belt, I’m now lecturing all over the country on the topic of LDN. This year, I’ve been invited to present our research data with Dr. Nicholas Palermo, DO at the 2019 LDN International Symposium as well as the Regional Osteopathic Medical Education (ROME) Conference about LDN. If you plan to attend, follow us on Facebook or Instagram and let us know you will be there or to set up a meeting with myself. If your organization or university would like to host Pioneer Health Center to present on LDN, please contact us here. Everyone knows what pain is because we’ve all experienced it. Pain is a signal from the body that something is wrong — an injury, damage, or maybe even an infection. This damage sends an impulse to the brain, which produces a pain response in the body.
This was the definition of pain during my formal training, but since then, it has become increasingly clear that while it may be accurate for acute pain, it’s not as accurate for chronic pain. Recent discoveries have shed light on how chronic pain differs from acute pain and why chronic pain is so difficult to treat. Until recently, chronic pain has been treated the same as acute pain, but it’s clear today that this approach does not work. In this two-part series, I’ll explain the challenge with chronic pain, new research on the subject, and new treatment options. Acute vs. Chronic PainAcute pain typically has a known cause and seems to serve a purpose. It alerts us to a problem, which gives us an opportunity to find a remedy. It usually subsides in a short time with or without treatment, rarely lasts longer than a few weeks or months, and disappears when the underlying cause is resolved. Chronic pain, on the other hand, can be entirely different. It generally serves no purpose in the body and may or may not have a known cause. Often, it can get worse for no apparent reason. Pain Without an Identifiable CauseCurrent research has revealed that in most cases of chronic pain, there are changes in the nervous system that alter the way the nerves function. These changes allow for the transmission of a pain signal from the brain without a corresponding input. In other words, we can experience pain without an identifiable cause and it can persist long after the injury heals. A classic example is a condition known as “phantom limb pain” where a patient who has had an amputation complains of pain in a limb that no longer exists. Another example is a condition called “post-herpetic neuralgia”. This occurs in a patient who has had a recent shingles outbreak and the severe debilitating pain persists long after the shingles has disappeared, perhaps even for years. These are “accepted” forms of chronic pain where we have a clue as to the cause of the initial pain. The real problem is when a patient continues to have severe pain after an injury has healed, or even worse, who never had an identifiable injury to begin with. There isn’t any measurable way to make a diagnosis. Yet doctors justify using pain medications, especially narcotics, in these cases. How many patients have been treated for their acute pain injury with narcotics and then told that the injury should have healed and they no longer need pain medication, yet the pain persists? And how many patients experiencing real pain are sent to a psychiatrist because no physical pain cause could be found so it’s “all in their head”? One of the biggest difficulties in identifying and treating pain has been that pain is purely subjective, meaning it can’t be physically measured and can only be quantified based on how the patient says they feel. When we actually look below the surface of pain, an entirely different picture emerges. That’s why conventional medicine has been failing miserably in its ability to effectively treat pain. Advancements in Identifying the Source of Chronic PainScientists have recently documented actual changes in the nervous system, especially in an area of the spinal cord known as the dorsal root ganglion, in which physiological changes have been identified in chronic pain conditions even when there is no known cause for the pain. These abnormalities include decreases or increases in certain chemicals, over-activation of certain nerve pathways, and involvement of nerves previously not associated with pain. With this new research, our understanding of acute and chronic pain is changing. This new data provides supporting evidence for the use of many other drugs and therapies in the treatment of pain beyond the “normal” pain meds. The Problem with Conventional Pain TreatmentHistorically, pain was treated based on its cause, location, and severity. The most popular pain assessment tool was the 0 to 10 scale where 0 was no pain and 10 is the most pain. Mild pains and headaches were treated with Aspirin, Acetaminophen, or Ibuprofen. When there is a more severe pain, stronger medications like opioids were used. Opioids are among the oldest known drugs and have been the standard of pain treatment for a very long time, and they’ve been used and abused for centuries. Used” refers to their medicinal properties in which they bind to receptors in the body referred to as opioid receptors, and thus block the sensation of pain. That is, they interfere with the impulse and response somewhere in the central nervous system — or so we used to think. “Abused” refers to the non-medical use in which they are used for their hallucinogenic or euphoric properties. The thinking was the more severe the pain the stronger the narcotic, but the 0 to 10 method is flawed and not always a proper assessment of pain. 30% of the U.S. Suffers from Chronic PainAccording to the Institute of Medicine of the National Academies Report, in 2011, over 100 million adult Americans had chronic pain. This estimate didn’t include acute pain or children. The entire population is estimated to be about 311 million people, or almost one-third of the U.S. population. That’s more than those suffering from diabetes (25.8 million), coronary heart disease (16.3 million), stroke (7 million) and cancer (11.9 million). This same report estimates that the cost to treat pain in the U.S. is between $560 and $635 billion a year. To say that we are dealing with an epidemic of chronic pain is an understatement. And the picture looks even worse when we look at the effectiveness of treatment. The Worst FactA 2002 Review published in The Clinical Journal of Pain revealed that, “None of the currently available treatments eliminates pain for the majority of patients.” This may be the saddest, most concerning fact of all. Report after report indicates that many pain patients, unhappy with the lack of success of therapy, tend to visit multiple physicians in search of a solution to their pain. We have a standard of care in which patients diagnosed with pain are routinely prescribed addictive drugs classified as narcotics that usually don’t work, at least not completely. So, patients seek another doctor or attempt another medication because they are still in pain. This system not only encourages drug-seeking behavior, it creates it. Patients whose only goal, at least originally, was to seek pain relief are now caught in a Catch 22 situation. Their desire to pursue pain relief has resulted in a social stigma so catastrophic that it, in addition to their pain, can destroy their lives. This problem is very real and could be one of the most significant silent catastrophes of our time. The Black SheepWe don’t hear about this silent epidemic the same way we hear about cancer, Alzheimer’s disease, Multiple Sclerosis or any other of the so-called accepted diseases. Chronic pain is like the black sheep that nobody wants to talk about. Many doctors and pharmacists are shying away from even treating chronic pain patients because of their fear of government regulators looking over their shoulder. These regulators are not necessarily concerned with proper patient treatment, but rather are searching for patterns of abuse. As mentioned earlier, how can we tell the difference between drug seeking for abuse and drug seeking for pain relief? Fear of loss of license and livelihood on the medical side is an absolute reality, which many patients don’t realize. Recent Advancements in TreatmentIn part two of this series, I will discuss recent advances in science and compounding pharmacy that are leading to customized pain therapy, producing results never seen before. Read Part 2: Compounding Pharmacy Advances Treatments in Chronic Pain, Reduces Opioid Epidemic. In part one of this two-part series on chronic pain, I discuss why chronic pain has become an epidemic and how conventional treatments are failing to address it. The scope of this problem is so massive yet nobody is talking about it. Who would have known that with all of our technology and science in a society as advanced as ours that we’re so inefficient at chronic pain treatment, which has led to this silent catastrophe?
The fact that almost one-third of the American population is impacted by chronic pain is shocking — not to mention the financial burden, estimated at more than $500 billion a year. It’s clear that our current understanding and beliefs about conventional pain therapies are not accurate and are in need of a re-examination. Through studying the most current literature and learning about the nature of pain, combined with our ability to customize medications as we do in compounding pharmacy, we have been able to provide new and unique options in chronic pain treatment. This, coupled with the education and tools provided to us by experts like Maureen Carling, RN, has provided the foundation for extraordinary experiences chronic pain treatment, resulting in significant relief in the vast majority of our patients as well as a dramatic decrease in opioid use. Compounding Pharmacy is Changing Chronic Pain TreatmentCompounding pharmacists are a specialized group of experts within the pharmacy field. Through the use of innovative equipment and pure pharmaceutical ingredients, we’re able to create customized medication therapies to help patients solve their unique needs. By customizing drug therapy, our goal is to create a treatment that enhances the therapeutic outcome while at the same time reduces the incidence of side effects. One such advancement is the development of transdermal bases, allowing the transport of medicines through the skin in order to deliver medications to a specific area of the body. This bypasses the digestive system altogether, giving the medication a much higher chance of getting to where we need it to go. I had been using transdermal treatments for various types of chronic pain conditions in my 15 years as a compounding pharmacist, but it wasn’t until I met Maureen Carling at a pain conference that our experience became quite extraordinary. The Most Accurate Assessment for PainIn 1994, Maureen developed and published an algorithm for the accurate assessment of pain. At that time, she was the pain management coordinator for the Riverside Regional Medical Center in Virginia. Maureen explained, “Without an accurate assessment of the pain, we are just shooting in the dark.” That is, if we don’t properly assess the pain to identify exactly which type of pain we are treating, how can we know which medications to choose for treatment? Over and over again, we hear of patients on very strong narcotics report that in spite of their drug therapy, they are still in pain. So, physicians increase their dose, yet there is still no reduction in pain. A year after she introduced her system of assessment, (called The Carling Method), the amount of morphine being used in the hospice program in Virginia decreased by 50% and the number of PCA pumps being used decreased by 75%. Maureen’s algorithm identifies eight different types, or classifications, of pain. Each type of pain is unique and has its own characteristics. An example of this is burning pain versus sharp, stabbing pain. We know that they’re not the same, but conventional medicine doesn’t address that — especially when it comes to choosing a treatment. This is one of the biggest problems in conventional pain management — treatment is based off a zero to ten scale based on how severe it is, not what kind it is. This only determines how much medication to give, not what medication is appropriate. Maureen’s algorithm is about identifying the type of pain so that we can choose the right type of therapy. Oftentimes, it’s not an opioid. One of the most significant differences among the types of pain is the fact that certain pains don’t completely respond to the opioids and some don’t respond at all. In fact, Maureen found that only two types of pain will fully respond to opioids. This fact along sheds much light on the huge problem of our conventional pain therapy. We were taught to prescribe opiates based on the severity of pain, not on the type of pain. We were never taught about different types of pain or that opioid resistance even existed. This new understanding completely changed my understanding of pain. A Case StudyA recent patient experience exemplifies this situation. We will call her “Sue”. A physician referred Sue to us shortly after being admitted to the hospital with an apparent Oxycontin overdose, which was prescribed following a surgical implantation of mesh in her lower abdomen. We were able to formulate a topical pain gel based on an assessment of her pain. We dispensed this prescription to her on a Friday as she was discharged. On Monday, I called to reassess the situation and Sue told us that the pain was “completely gone”. Most patients don’t respond that quickly and we often find that the longer someone has been in pain, the longer the process of pain relief is. Sue’s example exemplifies that when the appropriate medicines are used and properly titrated, the results can be remarkable. Not only does this result in true pain relief, but we are also seeing a consistent reduction in opioid use. Customizing Pain TreatmentWe currently have 20 to 30 different medication options that we can choose from to customize a pain gel. By accurately identifying the types of pain, we can now more accurately choose the appropriate combination of medications that would best treat a particular patients’ pains. Current research states that one-third of pain patients are dealing with four or more types of pain. As you can imagine, it can be quite complicated to treat this, yet the assessment tool developed by Maureen allows us to systematically and scientifically choose the most appropriate medications unique to that individual. Our ability to compound these drugs into a transdermal pain gel and deliver them to the targeted area has been shown to increase the effectiveness of the chronic pain treatment, and at the same time, significantly reduce the incidence of side effects. Moving Patients ForwardThe Carling Method includes a process whereby we can reassess the patient and titrate the medication by calibrating the gel and the opioid. During the re-assessment, we can now use the 0-10 scale to determine how well a medication is working and then appropriately titrate the dose based on our findings. It may take many weeks of re-assessing and recalibrating, but eventually, we almost always achieve significant pain relief and in many cases “pain-free”, with very little side effects and a corresponding reduction in opioid use. Is this not the desired outcome? My experience using the pain management process has been nothing short of amazing. Our biggest obstacle has been the difficulty in sharing and educating the medical community. I value the opportunity to speak to physician groups and patients about chronic pain treatment. If you are interested in having me speak at an upcoming event, please get in touch here. If you are a physician interested in collaborating with us on these new pain management techniques, contact us here. And if you are a patient with questions about your pain management treatment and would like a recommendation for a physician, don’t hesitate to reach out to us. Did you know that you’re made up of more bacteria cells than human cells? It’s true. This means it’s absolutely vital to nourish these cells to sustain good health. Today, however, our beneficial bacteria levels are threatened by substances like antibiotics, herbicides, pesticides, even birth control, and other powerful medications, inflammatory and toxic foods, and stress. Since a large majority of this bacteria lies within our digestive tract, that means in order to not only have good digestion but good overall health, we need to take good care of our guts. And considering the fact that about 80 percent of our immune cells lie in or around our digestive tract, we also need happy bacteria in order to have a strong immune system.
Dysbiosis, which is a microbial imbalance often caused by low probiotic counts, an imbalance of good to bad bacteria, a bacterial infection, or all the above, has been linked to digestive disorders, autoimmune diseases (i.e. rheumatoid arthritis, Hashimoto’s thyroiditis, lupus, multiple sclerosis (MS), diabetes, etc.), and even eczema. As the wise physician and founder of medicine, Hippocrates stated, “All disease begins in the gut”. We’ll add that all health can begin in the gut, too, if you treat it right. This is where probiotics come in. One of the best ways to nurture the beneficial bacteria, probiotics are gut bacteria that help your body produce and absorb nutrients and fight infection. Probiotics have been shown to improve dysbiosis as well as irritable bowel syndrome, antibiotic-associated diarrhea, and vaginal and urinary infections in women. There is also new evidence that probiotics may be able to help with autism, weight loss, depression and anxiety, neurological conditions such as Alzheimer’s, and other seemingly non-gut related conditions. Here at Pioneer Health Center, we understand the importance of a healthy gut microbiome, which is why we carry many oral probiotics as well as probiotic suppositories. Our pharmacist is certified in functional medicine, so we are able to get the best researched and quality line probiotics for our clients that aren’t always available at other locations. If you have a hunch your beneficial bacteria levels are off and would like to get tested and work with a certified expert in this field to get your probiotic count up and digestion improved, consider joining The Pioneer Assessment program, where you’ll go through a 4-month Heal Your Gut program, run lab tests and get direct guidance from our functional medicine expert and founder, Gene Gresh. |
|